Explore the essential information about tuberculosis – its causes, symptoms, diagnostic methods, and treatment. Learn about the global impact of TB and the efforts to combat this infectious disease.
Although it most commonly affects the respiratory system, tuberculosis (TB) is an infectious sickness that can affect any body area. Tuberculosis, caused by the bacteria Mycobacterium tuberculosis, continues to be a significant worldwide health issue.
Understanding Tuberculosis and Why it Happens?
Causes:
The bacteria Mycobacterium tuberculosis causes TB.
This contagious respiratory illness is transmitted through airborne particles released when an infected individual coughs, sneezes, speaks, or sings.
Transmission:
Tuberculosis (TB) is mainly spread through airborne transmission, occurring when an infected individual expels bacteria through coughing, sneezing, speaking, or singing.
People nearby can inhale these bacteria and become infected.
Close and prolonged contact with an infected person increases the risk of transmission.
TB is not easily spread through casual contact, such as shaking hands, sharing food or drink, or touching surfaces.
Factors such as poor ventilation, crowded living conditions, and prolonged close contact increase the risk of transmission.
Risk Factors:
Infected people with impaired immune systems are at a higher risk of developing tuberculosis (TB) sickness.
Risk factors for TB infection and progression to active disease include HIV infection, malnutrition, substance abuse, diabetes, certain medications (such as corticosteroids or chemotherapy), and conditions that weaken the immune system.
People living in areas with high TB prevalence or who have travelled to or migrated from such areas are at increased risk.
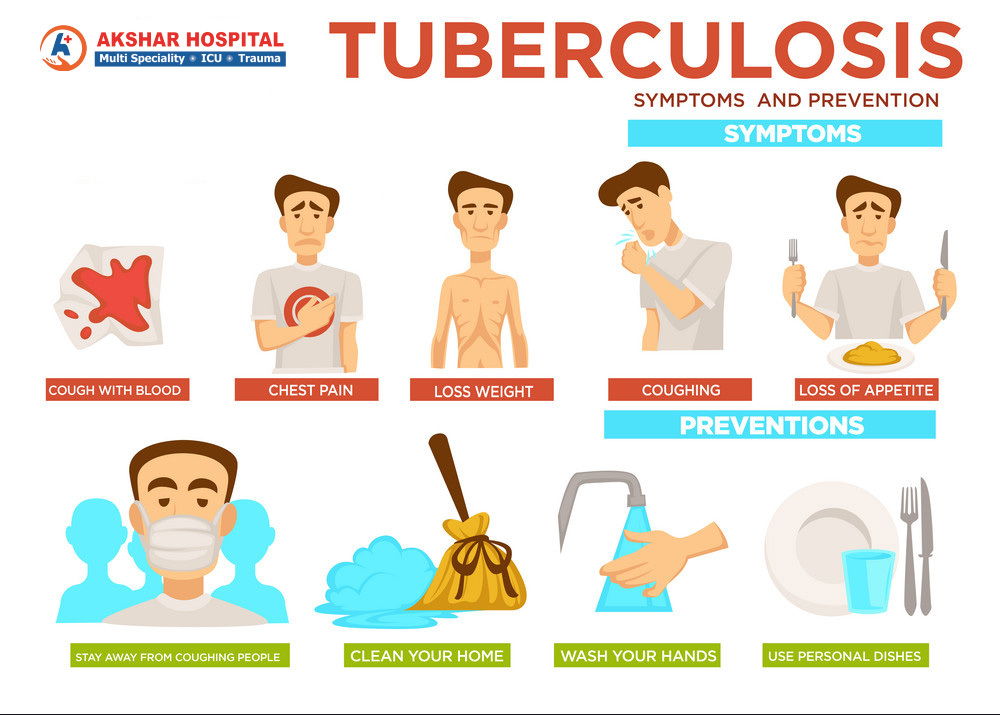
Prevention and Control:
The main goals of tuberculosis (TB) prevention are detecting and treating latent infections to stop them from becoming active diseases and promptly diagnosing and treating active diseases to stop them from spreading.
TB control measures include promptly identifying and treating active cases, contact tracing to identify and test people who may have been exposed to TB, encouraging the implementation of infection control measures at healthcare facilities and other high-risk areas, and administering preventative therapy to those who are at high risk of getting an active disease.
Symptoms of Tuberculosis:
Chronic Cough: Coughing up blood for over three weeks is a telltale sign of active tuberculosis.
Coughing up Blood or Sputum: Coughing that produces blood or pink-tinged sputum is known as hemoptysis and can be a sign of advanced TB.
Chest Pain: Anxiety or pain in the chest, particularly during coughing or breathing, may occur.
Fatigue: General weakness and fatigue can persist, even after adequate rest.
Weight Loss: Active tuberculosis often manifests as unexplained weight loss.
Loss of Appetite: A decrease in appetite leading to weight loss is often observed.
Fever and Night Sweats: Persistent low-grade fever and night sweats are typical symptoms.
Shortness of Breath: A common symptom, especially as the illness progresses, is having problems breathing or experiencing shortness of breath.
Swelling of Lymph Nodes: Enlarged and tender lymph nodes, especially in the neck, are possible.
Pulmonary Symptoms: Symptoms specific to pulmonary TB may include difficulty breathing, chest tightness, and wheezing.
Certain conditions can increase an individual's risk for tuberculosis disease:
- Diabetes (High Blood Sugar)
- Weakened Immune System (For example, HIV or AIDS)
- Being Malnourished
- Tobacco Use
Diagnosis of Tuberculosis:
Here are the key steps and methods commonly used in the diagnosis of TB:
Clinical Evaluation: A healthcare professional will assess the patient's medical history, symptoms, and risk factors for TB. Factors such as recent travel to high TB-prevalent areas, close contact with an individual with TB, and immunocompromised status are considered.
Physical Examination: Abnormal lung sounds, swollen lymph nodes, and other clinical abnormalities can be checked for during a physical examination.
Tuberculin Skin Testing (TST)/Interferon-Gamma Release Assay (IGRA): These tests help identify individuals with latent TB infection. A small amount of tuberculin is injected under the skin (TST), or blood is drawn to measure interferon-gamma release by T cells in response to TB antigens (IGRA).
Chest X-ray: One way to check for lung issues is via a chest X-ray, such as lung infiltrates or cavities, which suggest active pulmonary TB.
Sputum Analysis: Microscopic examination and culture of the patient's sputum are crucial for confirming the diagnosis of active pulmonary TB. Part of this process is taking a sample of the patient's sputum and testing it for Mycobacterium tuberculosis.
GeneXpert MTB/RIF Test: This molecular test helps detect the presence of TB bacteria and determine their susceptibility to the antibiotic rifampin. It is beneficial in diagnosing drug-resistant TB.
Biopsy or Other Imaging Studies: In some cases, a biopsy of affected tissue or additional imaging studies, like a CT scan, may be necessary for diagnosis, especially when extrapulmonary TB is suspected.
Blood Tests: Blood tests, such as the QuantiFERON-TB Gold test, may be used as an alternative to the tuberculin skin test to detect latent TB infection.
Key Aspect of Tuberculosis Treatment:
Tuberculosis (TB) treatment involves a combination of antibiotics over a specific duration. The standard TB treatment is highly effective, but it requires strict adherence to the prescribed medication regimen. Here are the key aspects of TB treatment:
First-Line Anti-TB Drugs:
The most common and effective drugs for treating TB are isoniazid, rifampin, ethambutol, and pyrazinamide.
A combination of these drugs is used to prevent the development of drug-resistant strains of Mycobacterium tuberculosis.
A typical course of treatment may be anywhere from six months to nine months long.
Directly Observed Therapy (DOT):
Healthcare providers often use Directly Observed Therapy (DOT) to follow the prescription schedule correctly.
A healthcare provider or other qualified professional watches the patient take their prescription doses in DOT.
Monitoring and Follow-up:
Regular monitoring of the patient's response to treatment is crucial. This may involve clinical evaluations, sputum tests, chest X-rays, and other relevant tests.
Follow-up appointments are set up to monitor the patient's recovery and handle any issues that may arise.
Drug Resistance Testing:
If there is suspicion of drug-resistant TB, drug susceptibility testing (DST) is performed to identify the most effective medications.
Second-line drugs may be prescribed if resistance to first-line drugs is confirmed.
Treatment of Latent TB Infection:
Individuals with latent TB infection may be prescribed isoniazid or other medications to prevent the development of active TB disease.
In most cases, the time required to treat a latent tuberculosis infection is less than that needed to treat an active case.
Adherence to Medication:
Strict adherence to the prescribed medication regimen is crucial for successful treatment.
Missing doses or stopping treatment prematurely can lead to treatment failure, relapse, or the development of drug-resistant strains.
Management of Side Effects:
TB medications may have side effects, and healthcare providers need to manage these appropriately.
Common side effects include nausea, vomiting, liver toxicity, and vision changes.
Supportive Care:
Adequate nutrition and overall health are essential for the patient's recovery. Supportive care may include a well-balanced diet, vitamin supplementation, and addressing other medical conditions.
Preventing Tuberculosis:
Preventing tuberculosis (TB) involves a combination of strategies to reduce the transmission of Mycobacterium tuberculosis and manage latent TB infection. Here are critical measures for TB prevention:
Vaccination (BCG Vaccine):
The Bacille Calmette-Guérin (BCG) vaccination offers partial immunity against severe manifestations of tuberculosis, particularly in pediatric populations.
BCG vaccination is commonly given in countries with a high prevalence of TB. However, its effectiveness in preventing pulmonary TB in adults is variable.
Screening and Early Detection:
Swiftly identifying and treating individuals with active tuberculosis (TB) is imperative to avoid the transmission of the disease.
Individuals with symptoms of TB, especially those with risk factors, should seek medical attention for testing and diagnosis.
Contact Tracing:
Identifying and conducting tests on persons who have had close contact with a person diagnosed with active tuberculosis (TB) aids in the early detection and treatment of latent TB infection or active TB disease.
Treatment of Latent TB Infection:
Individuals with latent TB infection are at risk of developing active TB. Treating latent TB with medications, such as isoniazid, can prevent the progression to active disease.
Infection Control Measures:
Enforcing infection control protocols in healthcare facilities and other areas with a high risk of transmission can effectively mitigate the spread of tuberculosis.
This includes proper ventilation, use of respiratory protection for healthcare workers, and isolation of patients with active TB when necessary.
Education and Awareness:
Public education campaigns can raise awareness about TB, its symptoms, and the importance of seeking medical attention for diagnosis and treatment.
Promoting understanding of TB transmission modes and prevention measures is essential for community engagement.
Treatment Adherence Support:
Ensuring that individuals diagnosed with TB adhere to their prescribed medication regimen is crucial for successful treatment and preventing the development of drug-resistant strains.
Directly Observed Therapy (DOT) is a strategy where healthcare providers or trained individuals observe patients taking each dose of medication to enhance adherence.
Addressing Social Determinants:
Addressing social factors such as poverty, overcrowded living conditions, and lack of access to healthcare can contribute to TB prevention efforts.
Screening and Testing High-Risk Populations:
Targeted screening and testing of high-risk populations, such as those with HIV infection, substance use disorders, or recent immigrants from high TB-prevalence areas, can help identify and manage TB cases more effectively.
Global Collaboration:
TB prevention requires global collaboration and efforts to control the disease, especially in regions with high prevalence.
Research and development of new diagnostic tools, drugs, and vaccines are essential for advancing TB prevention efforts.
Frequently Asked Questions (FAQ)
Tuberculosis is caused by the bacterium Mycobacterium tuberculosis. It is primarily transmitted through the air when an infected person coughs, sneezes, or talks.
TB is primarily transmitted through the air. Nearby inhalation of germs occurs when an infected person sneezes or coughs. Factors such as weakened immune systems and crowded living conditions increase the risk of transmission.
Common symptoms of tuberculosis include a persistent cough, chest pain, fatigue, weight loss, fever, and night sweats. However, some individuals with TB may not exhibit any symptoms.
Diagnosis involves various methods, including tuberculin skin tests, blood tests, chest X-rays, and sputum tests. These assays help confirm the bacterium's existence and identify the infection latent versus active state.
Yes, tuberculosis is treatable with a combination of antibiotics over an extended period, typically six to nine months. Finishing all your medications is essential to prevent drug-resistant bacteria from emerging.
Preventing the spread of tuberculosis involves identifying and treating active cases promptly. Vaccination with the Bacillus Calmette-Guérin (BCG) vaccine is also recommended, especially in areas with a high prevalence of TB.
Yes, tuberculosis remains a significant global health concern, particularly in low-income and resource-limited settings. Efforts to control TB include improved diagnostics, treatment accessibility, and public health interventions.
Tuberculosis
Tuberculosis treatment involves a combination of antibiotics taken for several months to kill the bacteria causing the disease. Medication adherence is crucial to prevent drug resistance and ensure successful treatment.




